The widespread neglect of children with TB constitutes a human rights violation that demands urgent attention from the international community. The right to equal access to healthcare is enshrined in international human rights agreements, including the Convention on the Rights of the Child, the European Convention on Human Rights, the American Convention on Human Rights, and the African Charter on Human and Peoples’ Rights. Legal remedies should be a last resort, however, as timely action from both developing and donor countries can save millions of lives. At the same time recent precedents, including cases decided in national courts, have made it easier for legal activists to use human rights law to redress unequal access to healthcare.1,2
The widespread neglect of children with TB demands urgent attention from the international community.
Children are particularly vulnerable to TB. Children with TB are at high risk of developing severe forms of the disease and at high risk of dying – especially infants and children under five years of age. Furthermore, strong evidence of the effectiveness of TB prevention and treatment in children has been available for decades. However, in most countries affected by TB a substantial gap remains between policy guidelines, based on international and national recommendations, and actual practice.
Incident Cases Globally
Estimated number of incident cases aged 0-14 (2016)
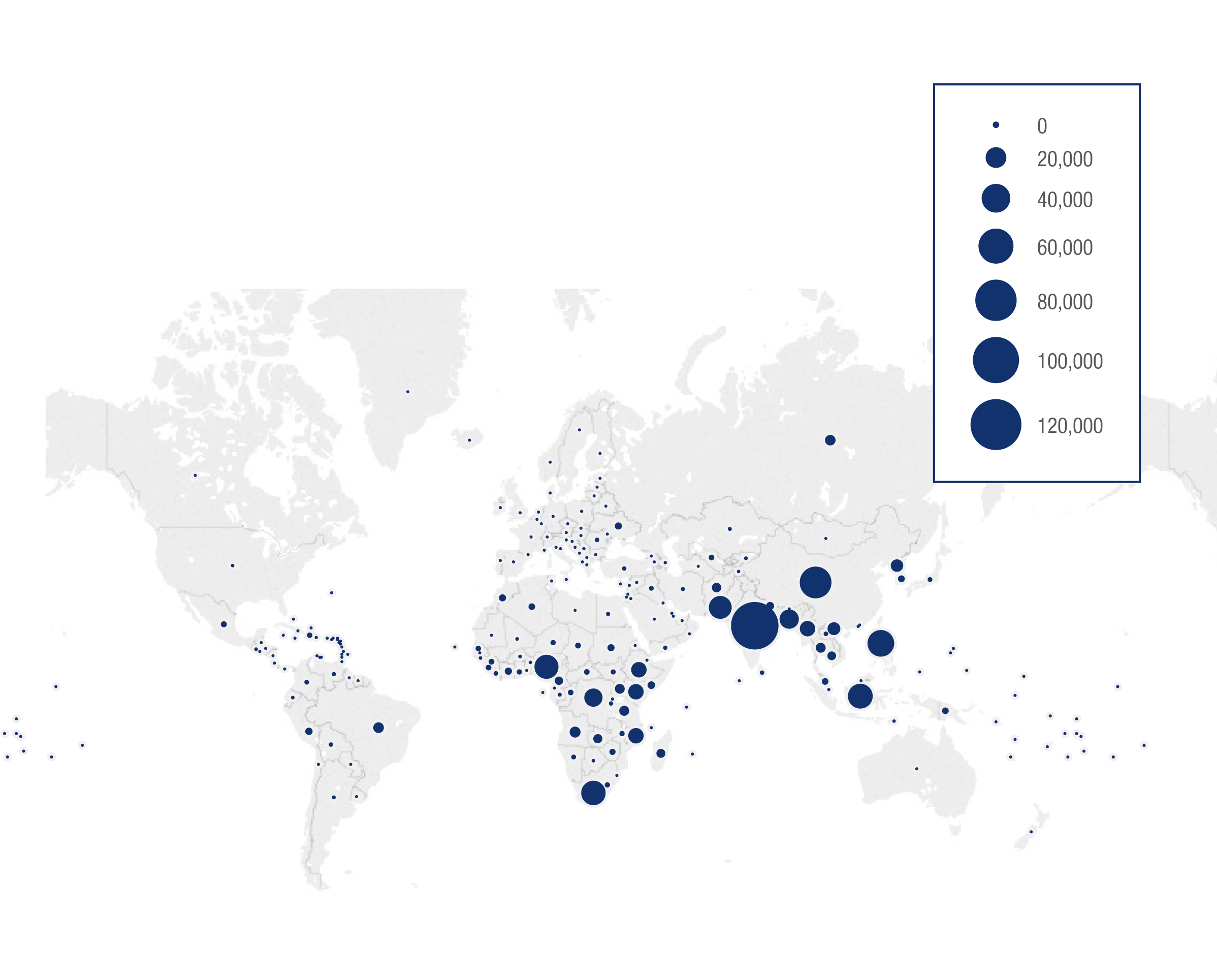
One major reason for this long-standing neglect is that children with TB, especially young children, are much less likely to be contagious than adolescents or adults with the disease.3,4,5 But if not detected and treated, they are more likely to develop severe disease and die. According to new research, around a million children worldwide develop active TB and 239,000 die every year, representing one in seven of all TB-related deaths.6 Children with TB die from the disease at disproportionate rates compared with adults, representing 10 percent of TB incidence but 16 percent of TB deaths globally.7,8 The burden of child TB is highest in low- and middle-income countries, where children may represent over a fifth of all cases.9,10 Immature immune systems make children more likely to develop severe forms of the disease, such as TB meningitis, disseminated TB, and TB of the bones and joints.
Most TB-related deaths in children occur in young children who have not been diagnosed or treated, representing a missed opportunity for prevention.11 The burden of multidrug-resistant TB (MDR-TB) in children is still largely unknown but it is estimated that less than 10 percent of all children with MDR-TB are detected and treated.12 As child mortality overall has fallen in many countries over the last 20 years, the continued neglect of TB in children has resulted in TB now being one of the major infectious diseases causing death in children globally, despite it being treatable and preventable. TB also has profound indirect consequences on child health as children are commonly orphaned or suffer the consequences of increasing poverty due to catastrophic costs to the family or household that are often associated with having TB.
Ending neglect of TB in children calls for tmore integrated, family-centred approaches to TB care and prevention, as well as engagement with the wider health sector including the maternal and child health sectors. Furthermore, there is major potential to make much more progress with the low-cost tools that we possess, including child contact screening and management – the standard of care in high-income, low TB burden countries, but which is rare in TB endemic countries. Contact screening requires a health worker to determine if any TB patient has contacts in the home, workplace, or even social environments, which are at risk of becoming infected with TB due to their proximity to the patient. A programme in the resource-limited, high TB-burden setting of Uganda has proven successful in increasing the detection of children with TB while, at the same time, dramatically increasing the numbers of children – who have been exposed to TB – receiving TB preventive therapy, with services delivered to whole families within their own communities.
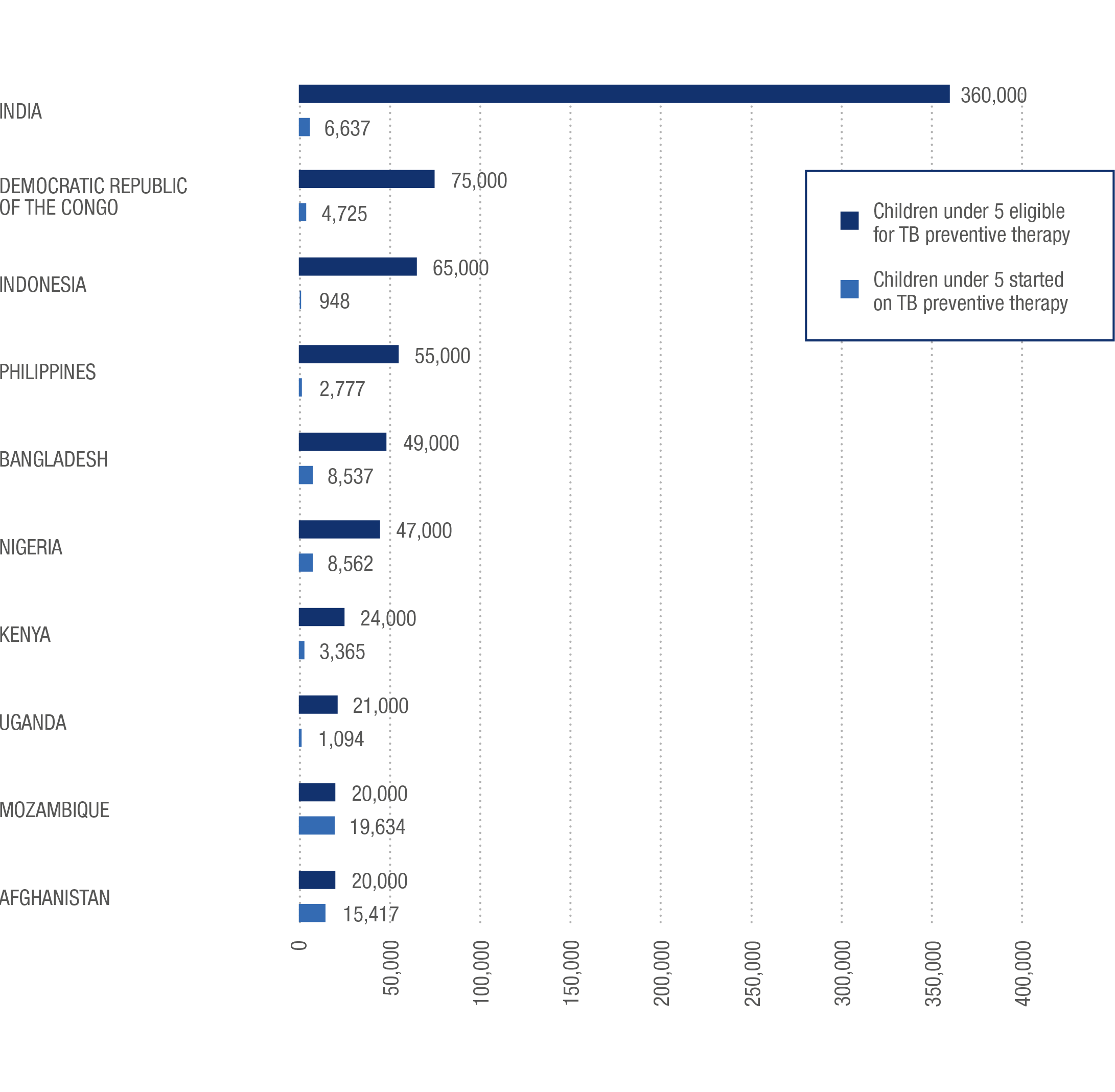
Children Eligible For And Started On TB Preventive Therapy
Top 10 Countries by Number Eligible
The fight against TB has reached a critical turning point. A concerted effort by the global public health community helped save more than 50 million lives from TB between 2000 and 2016, as global incidence fell by a third and the annual death toll fell by almost half over the same period.13,14 However, far greater efforts are required to end the global TB epidemic. The global End TB Strategy adopted in 2015 provided an unprecedented opportunity for the global health community to finally end the long-standing neglect of TB in children – but children with TB continue to be neglected in large numbers.
We must seize the opportunity. Millions of young lives hang in the balance.
Above all, ending the epidemic of child TB requires political will and, in this respect too, the fight against TB is at a turning point. On 26 September 2018, the United Nations will convene the first High-Level Meeting (HLM) on TB where heads of state and government will, for the first time ever, issue a political declaration on global TB. The political commitments that will be enshrined in this declaration have the potential to dramatically change the trajectory of the epidemic. The political commitments secured at previous UN High-Level Meetings on HIV/AIDS, non-communicable diseases and antimicrobial resistance have accelerated the response to those other global health challenges. The HLM on TB provides a historic opportunity to galvanise support for ending the child TB epidemic. We must seize the opportunity. Millions of young lives hang in the balance.
The Neglect of Child TB
Medical neglect of child TB has long been a generally acknowledged fact.15 Paediatric TB screening and treatment have improved greatly in the developed world, but neglect of child TB remains common in middle- and low-income countries, reflecting the special pathology of TB in children.16,17,18,19 In contrast to adults with active TB, children tend to have ‘pauci-bacillary TB’, meaning there are relatively few bacteria in the patient’s body, making them both less contagious and harder to diagnose. The bacteria are less likely to show up in sputum samples, further complicated by young children’s difficulty in producing sputum, yielding false negatives using the common acid-fast bacteria smear method. Children are less likely to develop lung lesions that show up on X-rays and, tests using fluid aspirated from the stomach, can be inaccurate and difficult to perform.20,21
“Children with TB are also less infectious than sick adults, prompting healthcare providers in many countries
to classify them as lower priority.”
Numbers of Children Who Became Sick With TB, 2016
Top 20 Countries (Estimated Number of Incident Cases Aged 0-14)
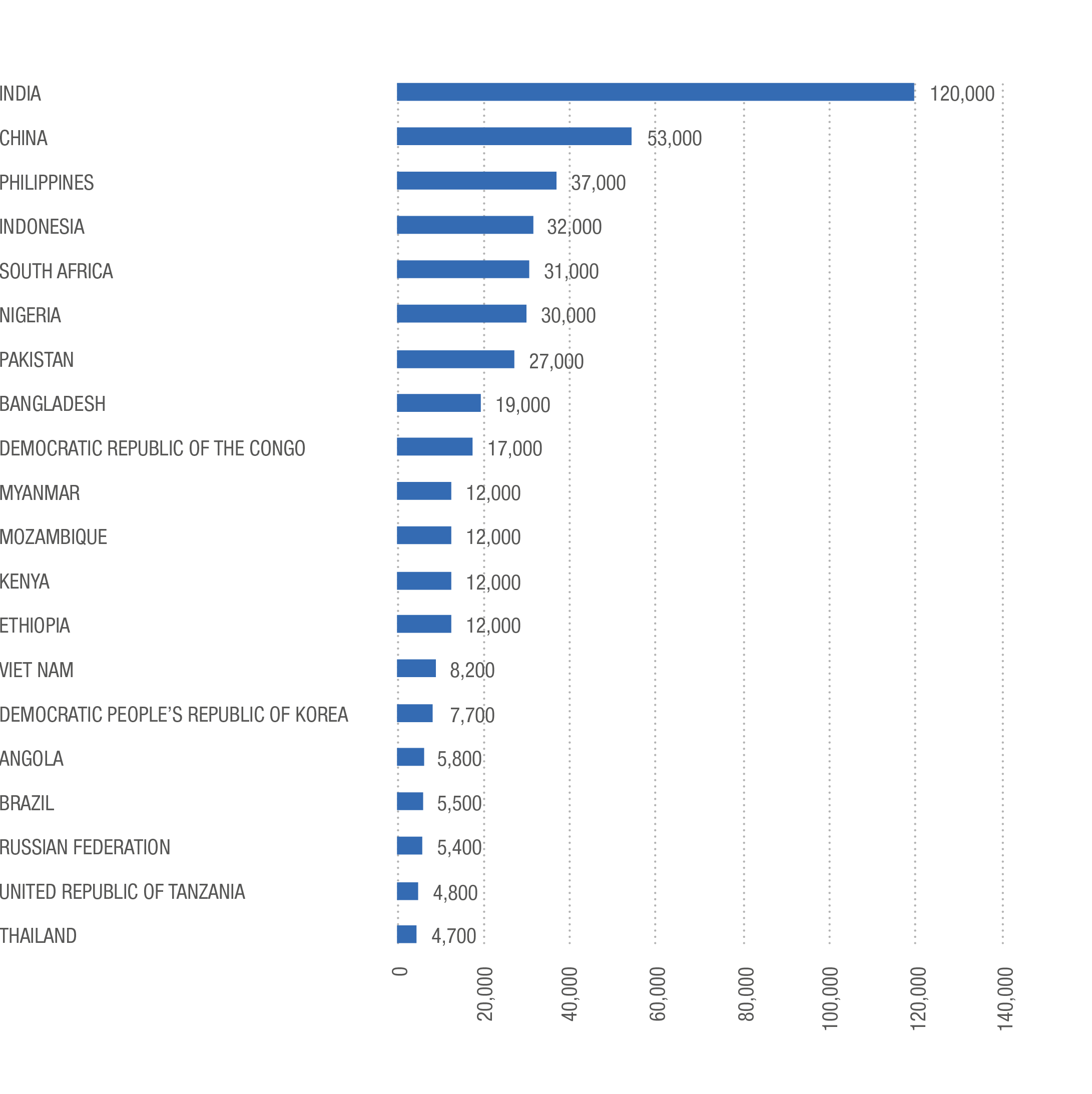
Because their bacterial burden is lower, children with TB are also less infectious than sick adults, prompting healthcare providers in many countries to classify them as lower priority.2223,24 But a policy of triage or rationing in this way only puts distance between vulnerable children and the care they need. Furthermore, a survey of 29 high-burden countries by Médecins sans Frontières (MSF) found just five countries were widely implementing child-friendly fixed dose combination therapy for TB as the standard of care25 while, according to the World Health Organization (WHO), just 13 percent of children eligible for preventive treatment with isoniazid receive it globally.26 However, children respond well to commonly used treatments, with less than one percent mortality among children treated for TB (rising to 13 percent for children with MDR-TB) suggesting nearly all deaths among children are preventable with appropriate action.27,28
Beyond the tragic loss of life, the continued neglect of paediatric TB is dangerously shortsighted as individuals who have been infected with TB bacilli in childhood may still grow into sick, infectious adults, worsening the long-term burden of the disease and undermining efforts to eliminate it.29